This is a case of 55 year old male who is construction worker(floor tile worker) by occupation and resident of olugonda of Nalgonda district who came with chief complaints of
- YELLOWISH DISCOLOURATION OF EYE SINCE 1 MONTH.
-FEVER SINCE 1 MONTH.
-LOSS OF APPETITE SINCE 20 days.
-PAIN IN THE ABDOMEN SINCE 20 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic a month ago then he noticed yellowish discolouration of eye for which he used HERBAL MEDICINE and then he complained of fever which was low grade and continuous type not associated with chills and rigours.
The patient later developed pain abdomen which was insidious in onset and gradually progressive. He localised the pain to his right upper quadrant. It was sharp in nature non radiating. There are no aggravating and relieving factors.
History of decreased appetite from 1 month.
History of itching over the legs since 1 month which was increased at evenings and night.
No history of loose stools, nausea, vomiting, headache, dizziness, burning micturition.
No history of Malena, constipation, abdominal distension and haemetemesis .
PAST HISTORY:
Patient is a known case of PULMONARY TUBERCULOSIS 25 years ago for which he used medication for 3 months.
Appendectomy 25 years back.
Not a known case of DM, HTN, CVA, CAD, Thyroid disorders, Asthma and epilepsy.
PERSONAL HISTORY:
Daily routine: He wakes up at 5 in the morning and freshens up. Have tea at 8 AM and goes to work by 9 in the morning. He takes lunch at 1:30 PM. Around 5 PM he comes back to his house.
He has dinner by 8 PM and goes to bed at 9:30 PM.
DIET: MIXED.
APPETITE: DECREASED SINCE 20 DAYS.
SLEEP: ADEQUATE.
BOWEL AND BLADDER: IRREGULAR
(once in 3 days and watery since 10 days)
ADDICTIONS: Alcohol since 35 years(180ML every day) and chews tobacco from when he was 25 years old. Stopped drinking alcohol 2 months back.
FAMILY HISTORY:
Not significant.
CLINICAL EXAMINATION:
GENERAL EXAMINATION:
I have examined the patient after taken prior consent and informing the patient. The examination was done in both supine and sitting position in a well lit room.
The patient was conscious coherent and cooperative. Well oriented to time place and person. Well built and nourished.
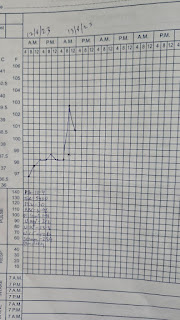
VITALS: BP:110/70mmHg
RR: 16 cycles/ min
PULSE RATE: 90 beats per min
Temp: 100 F
PALLOR: ABSENT.
ICTERUS: PRESENT.
CYANOSIS: ABSENT
CLUBBING: ABSENT
LYMPHADENOPATHY: NO
EDEMA: ABSENT.
SYSTEMATIC EXAMINATION:
1) PER ABDOMEN:
INSPECTION:
-Shape of abdomen: flat
-Umbilicus: inverted
-Presence of appendectomy scar
-All quadrants are moving equally with respiration
-No engorged veins
- skin over the abdomen is smooth.
PALPATION:
-No local rise of temperature
- diffuse tenderness over the abdomen
-No Rebound tenderness
-No guarding rigidity
- liver not palpable
- spleen not palpable
Abdominal girth: 89 cm
PERCUSSION:
Shifting dullness - absent
No fluid thrill
Liver span - 9 cm
Liver dullness is not heard at 5th intercostal space.
AUSCULTATION:
diminished bowel sounds
2) CARDIOVASCULAR:
Inspection:
apex beat :5th ICS half inch medial to midclavicular line
Palpation:
inspectory findings confirmed, No thrills or parasternal heave
Auscultation: S1 , S2 heard and no murmurs
3) RESPIRATORY SYSTEM:
INSPECTION:
Shape of chest:Bilaterally symmetrical, Elliptical in shape
No visible chest deformities
No kyphoscoliosis,
Abdomino thoracic respiration, No irregular respiration
No tracheal shift
No dropping of shoulders, Spino scapular distance appears equal on both sides
no sinuses and scars
No engorged veins
PALPATION
Inspectory findings confirmed by Palpation
Chest movements - normal
Chest expansion-equal on both sides
PERCUSSION:
Resonant note heard over all areas
AUSCULTATION:
- fine crepitations heard at right infra clavicular and right mammary areas.
- Norma vesicular breath sounds heard in all other areas.
-Vocal resonance: normal in all areas
4) CNS:
Higher mental functions :intact
Cranial nerves intact
Motor examination: R L
Bulk. N N
Tone. N N
Power. N N
Reflexes:
Biceps. 2+ 2+
Triceps. 2+ 2+
Supinator 2+. 2+
Knee 2+ 2+
Ankle. 2+. 2+
Sensory examination:Normal
No meningeal signs
PROVISIONAL DIAGNOSIS:
CHRONIC LIVER DISEASE? with HIV test reactive (Z +ve).
Hyponatremia under evaluation.
INVESTIGATIONS:
BLOOD UREA: Normal
total bilirubin: increased (1.26mg/dL)
Direct bilirubin: increased (0.30mg/dL)
SGOT(AST): elevated (88 IU/L)
SGPT(ALT): elevated (72 IU/L)
ALKALINE PHOSPHATASE: elevated ( 553 IU/L)
ALBUMIN: decreased (2.95g/dL)













Comments
Post a Comment